Diagnosis prediabetes? – Tips for people with prediabetes and those at high risk of developing type 2 diabetes. Learn how to prevent it here!
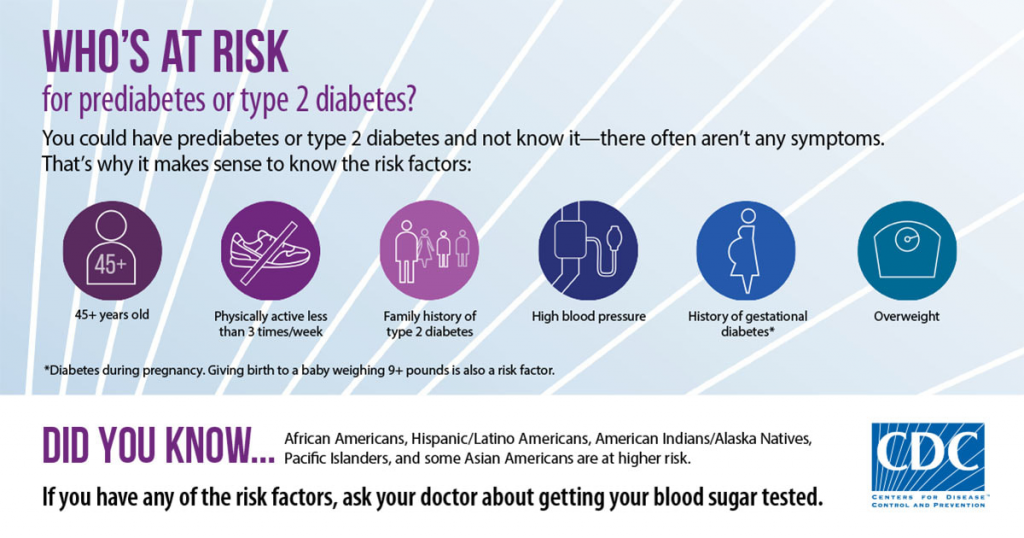
What are the contributing factors to Diabetes?
There are many contributing factors to diabetes; perhaps the biggest single contributor is if you are overweight or have a poor diet, other factors would include inadequate physical activity, high blood pressure, or even your age. The more contributing factors an individual has, the greater the risk, and then if there is also family history, risks increase further. The good news is that most of these contributing factors can be mitigated, reducing the overall risk.
LEARN ABOUT YOUR DIABETES MELLITUS RISKS – this is adapted/based on American Diabetes Association’s Diabetes Risk Test.
Tips to Prevent Type 2 Diabetes
There are many aspects to a healthy lifestyle; what constitutes healthy varies from person to person, depending on genetics. Despite this, there are some things that can be done that are effective for everyone. Below is a list of our favorites.
1. Have an Early Dinner
A new research study shows that eating dinner several hours before bedtime can reduce the risk of developing type 2 diabetes.
A team of researchers from Massachusetts General Hospital (MGH), Brigham and Women’s Hospital (BWH), and the University of Murcia in Spain conducted a clinical trial to understand the links between blood sugar and melatonin production. The pineal gland naturally secretes this hormone in the brain to regulate the day/night cycle.
The timing of meals during the day plays an important role in glycemic control, including, which should be spaced out timewise, and, if possible, always eaten at a fixed time.
The results show that participants’ blood melatonin levels were 3.5 times higher after a late dinner. A late dinner decreases insulin levels and, consequently, increases blood sugar. The effect of late eating impairing glucose tolerance was stronger in the MTNR1B G-allele carriers than in noncarriers.
2. Diabetes and Breakfast timing
In 2018 an American study analyzed data on the health and dietary intake of 10,574 US adults who enrolled in the National Health and Nutrition Examination Survey. It was found that having breakfast earlier rather than later (before 8:30 in the morning) can reduce insulin resistance, thereby reducing the risk of developing type 2 diabetes.
They found that insulin resistance was higher among those who ate over a shorter duration across the day (time-restricted eating) — and lower in all groups that began eating before 8.30 in the morning.
3. Diabetes and Fasting
Also, it’s important to note that diabetic people should always consult their physicians prior to starting intermittent fasting because they might need to adjust their insulin doses or other medications to avoid hypoglycemia or even hyperglycemia.
4. What to Eat to Prevent Diabetes
A low Glycemic index diet has been shown to delay or even prevent diabetes by preventing dangerous spikes in blood glucose levels. Here it’s worth noting that a precisely crafted diabetic meal plan does not differ from a healthy balanced meal plan which focuses on achieving a healthy weight with a balanced – nutritionally dense diet like the Mediterranean diet. The Glycemic index and the calculation of Glycemic load are helpful tools for those seeking to adapt to such a diet.
Balance is key and can be achieved by following simple food swaps/exchanges:
- Consume non-starchy vegetables.
- Minimize consumption of added sugars and refined grains.
- Choose whole foods vs. highly processed foods.
- Replace sugar-sweetened beverages with water.
Source: 2019 ADA Consensus Report by Todays Dietitian
Food Tracking is important because while a GI diet does help control diabetes, it can also increase the amount of fat and sugar alternatives in the diet, the tolerance of which is unpredictable due to the variability of gut fauna. By keeping a food diary, when problems arise, foods or ingredients can be identified more easily and excluded from the diet if needed. The DiabTrend app (for android or iPhone) assists with the tracking of food and displays the Glycemic index of many foods, so it’s the perfect app to keep track of your low GI diet.
5. Enjoy Spices with Food
There is evidence that consuming various spices during a meal reduces blood glucose levels below what they would otherwise have been in prediabetes and type 2 diabetes. Although the mechanism is still not 100% clear, it could be due to either improving beta-cell functions or insulin sensitization.
6. What to Drink to Prevent Type 2 Diabetes
There are numerous studies that show that caffeine impacts blood glucose levels; however, its effects vary greatly from person to person, either increasing or decreasing blood sugar levels, often depending on when you consume it in relation to meals. Some experimentation is needed to determine what works for you.
Note: for some people, it does not affect blood glucose.
Plain old water is good for diabetics because it has a neutral effect on blood glucose levels, whereas low-fat milk contains many other nutrients such as protein and calcium, making it a good option. That being said, it still has simple carbohydrates that should be counted towards your daily allowance.
Note: drinking milk could result in a blood sugar spike for some people, especially in the morning, even though it has a low Glycemic index.
7. Food Tracking with a Food Diary to Prevent Type 2 Diabetes
The information above about the impact of specific foods and drinks on blood sugar levels is an important example of why dietary tracking is essential for everyone, not just for diabetics. In the case of prediabetes or type 2 diabetes, you need to test what works well for your particular case to determine what you should consume and when to do so, i.e. before or after eating, morning or evening, etc. A smartphone application such as DiabTrend is a great tool for managing dietary intake.
8. Exercise Directly After Eating to prevent type 2 Diabetes
The tradition of walking after eating is an age-old practice maintained because we feel better when we do so, especially if a meal makes you feel sleepy afterward.
Exactly when you should exercise depends on the type of carbohydrates (different carbohydrates are digested at different rates) in the food. Still, ultimately it’s about how you feel, but the study suggests around 30 minutes after eating.
In terms of the type of exercise, swimming and marathon running are probably a bad idea along with any extreme exercise routine. We suggest perhaps cycling or walking.
As an additional benefit of exercise, less blood sugar results in less sugar converted into glycogen or fat in the liver.
9. Take an Ice Bath After Eating to Prevent Type 2 Diabetes!
In type 2 diabetic patients a cold exposure (10-15°C) is suggested to improve glycemic control, through activating brown adipose tissue and also improving insulin sensitivity. However, people with diabetes need to be careful with ice baths as they are associated with reduced ability to maintain a core temperature in extreme temperature changes.
10. Relax, Reduce Stress to Prevent Diabetes.
Avoid hearing any bad news and shocks after eating! Adrenaline increases blood glucose levels, which, when combined with the higher blood glucose levels after a meal, can cause a dangerous spike and potentially cause damage to your body.
Wrapping Up
These tips and tricks mentioned in the article have one aim in mind: to keep your blood sugar levels and body weight in a healthy range. And the best way to do this is to have a healthy balanced diet and an active lifestyle. It’s tough breaking old habits, there are no quick fixes, but some simple things can be done, added to your diet and lifestyle that will help, such as those listed above.